Understanding Cognitive Behavioural Therapy (CBT)
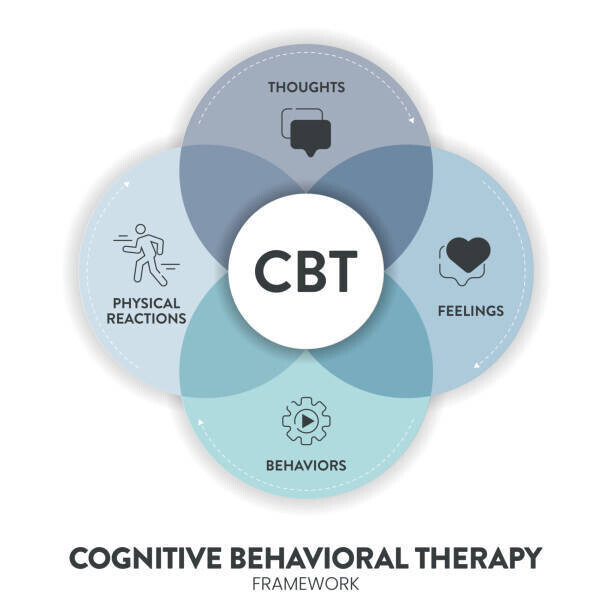
Cognitive Behavioural Therapy (CBT) is a psychological treatment that has been shown to improve mental health for people experiencing a wide range of difficulties. It is a dynamic approach that works across cultures, age groups and also supports sexual and gender minority individuals (Martell, 2004). CBT is recommended for people with mental health problems (Compton et al., 2004) and focuses on identifying, evaluating, and changing unhelpful thoughts and behaviours.
CBT can also be adapted for people from specific cultural backgrounds or for those with mild learning difficulties. In cases where someone has multiple diagnoses, cognitive restructuring can be combined with exposure therapy to help challenge and correct negative expectations about facing fears. Research shows that cognitive restructuring is effective for many anxiety-related disorders (Safren & Heimberg, 1998).
CBT is a structured, collaborative approach that focuses on the present. It helps individuals manage their own mental health, act as their own therapist, and improve overall wellbeing. It is recommended by the National Institute for Health and Clinical Excellence (NICE) for many emotional health problems.
Although the name “Cognitive Behavioural Therapy” may sound complicated, it is a practical, structured, problem-solving approach. Scientific research has shown it can help with anxiety, post-traumatic stress, obsessive-compulsive disorder, low mood, and depression (National Institute for Health and Clinical Excellence, 2005; Beck, 1993; Hoffman & Smits, 2008). Studies also show that CBT can significantly improve functioning and overall quality of life.
CBT is usually a short-term therapy that focuses on behaviour and thinking patterns. It helps people understand their stressors and think more rationally about the causes of anxiety. Developed by Aaron Beck in the early 1960s, CBT quickly became one of the leading psychological therapies in Western countries, used widely in both mental health and medical practice. Its popularity and effectiveness come from the strong connection between theory and practice, which has been proven in many scientific studies for treating disorders such as depression and anxiety.